Trichomoniasis is a common sexually transmitted infection (STI) caused by a parasite that spreads through sexual contact. Although some people with trichomoniasis experience symptoms, many are asymptomatic. The infection requires special attention during pregnancy due to its potential complications. However, with timely diagnosis, proper treatment, and effective prevention methods, the infection can be cured and prevented from coming back. In this article, you’ll learn about what causes trichomoniasis, how it manifests in the body, how testing works, and which treatments can help you recover.
What Is Trichomoniasis?
Trichomoniasis, sometimes referred to as “trich,” is a parasitic infection that occurs in the genital and urinary tract. While easily treated with medication, it can cause uncomfortable symptoms and increase the risk of contracting other STIs, such as HIV. Since most people carrying trichomoniasis don’t develop any visible signs of the disease, they may unknowingly carry and transmit the infection.
Trichomoniasis is spread during sex through genital contact. The parasite can be spread through infected vaginal fluids or semen during vaginal, anal, manual, and oral sex. Trichomoniasis is also spread by sharing sex toys that are not properly washed between uses. However, trichomoniasis is not transmitted through casual contact such as sharing food, kissing, or hugging.
Symptoms of Trichomoniasis
Many people infected with trichomoniasis never realize they have it. According to the CDC, at least 70% of infected individuals have little to no genital symptoms of trichomoniasis, yet they are still capable of transmitting the infection to their partners. When symptoms do appear, they typically show up between 5 to 28 days after exposure and may come and go.
Symptoms in Females
Trichomoniasis symptoms are more commonly seen in females than in males. Some common symptoms in females include:
- Vaginal Itching, Burning, and Redness: The infection can cause itching and soreness in the vaginal area. The area may become red, inflamed, and sensitive to the touch. Sometimes, the itching can spread to the inner parts of the thighs as well.
- Foul-Smelling Vaginal Discharge: Females may notice an unusual amount of vaginal discharge that is foamy or thin. The discharge can be clear, white, gray, yellow, or green and may have an unpleasant fishy smell.
- Pain During Urination or Intercourse: The infection may cause a burning sensation during urination. Sex can become painful or uncomfortable. For some, these symptoms are not very severe, but for others, they can be extremely painful.
Symptoms in Males
Most males with trichomoniasis have no symptoms or only mild symptoms, but they can still pass the infection on to their partners. If symptoms do appear, they typically include:
- Burning During Urination and Ejaculation: The infection may cause burning when urinating or ejaculating. The level of discomfort can vary from one individual to the next.
- Discharge From the Penis: The infection can cause penile discharge. The discharge can be white in color and frothy or thin in texture.
- Irritation or Itching Inside the Penis: The infection can cause pain around the foreskin or head of the penis. The area may also turn red and get swollen.
Causes of Trichomoniasis
Trichomoniasis is caused by a tiny parasite called Trichomonas vaginalis. Once infected, you can spread it to others through:
Unprotected Sexual Contact
Trichomoniasis is spread primarily through genital-to-genital contact during unprotected sex. It most commonly infects the vagina, cervix, and urethra in females, while males may experience infection in the urethra and sometimes the prostate.
Sharing Sex Toys
Sex toys can spread the parasite from one person to another if they are not cleaned thoroughly after every use. This is less common than transmission by direct sexual contact but remains a significant risk. Putting fresh condoms on toys or cleaning them can prevent this type of transmission.
Infection During Pregnancy
Infants can be infected with trichomoniasis as they pass through the birth canal. However, this is very rare. Pregnant women can take antibiotics to clear the infection before giving birth. If you notice symptoms of trichomoniasis while pregnant, you should contact your doctor immediately.
Risk Factors for Trichomoniasis
Trichomoniasis can affect anyone, and your risk of catching it increases if you have:
Multiple Sexual Partners
Having multiple sexual partners puts you at an increased risk of encountering a person who has trichomoniasis. However, it’s important to note that any sexually active individual can be infected with trichomoniasis-even a person with only one sexual partner.
Prior STIs
People who have had other STIs may have inflamed or blistered genitals that are more susceptible to new infections. Inflammation from previous STIs can create tiny breaks in skin tissue where the parasite that causes trichomoniasis can settle. Research shows that having one STI significantly increases the risk of getting another.
Testing for Trichomoniasis
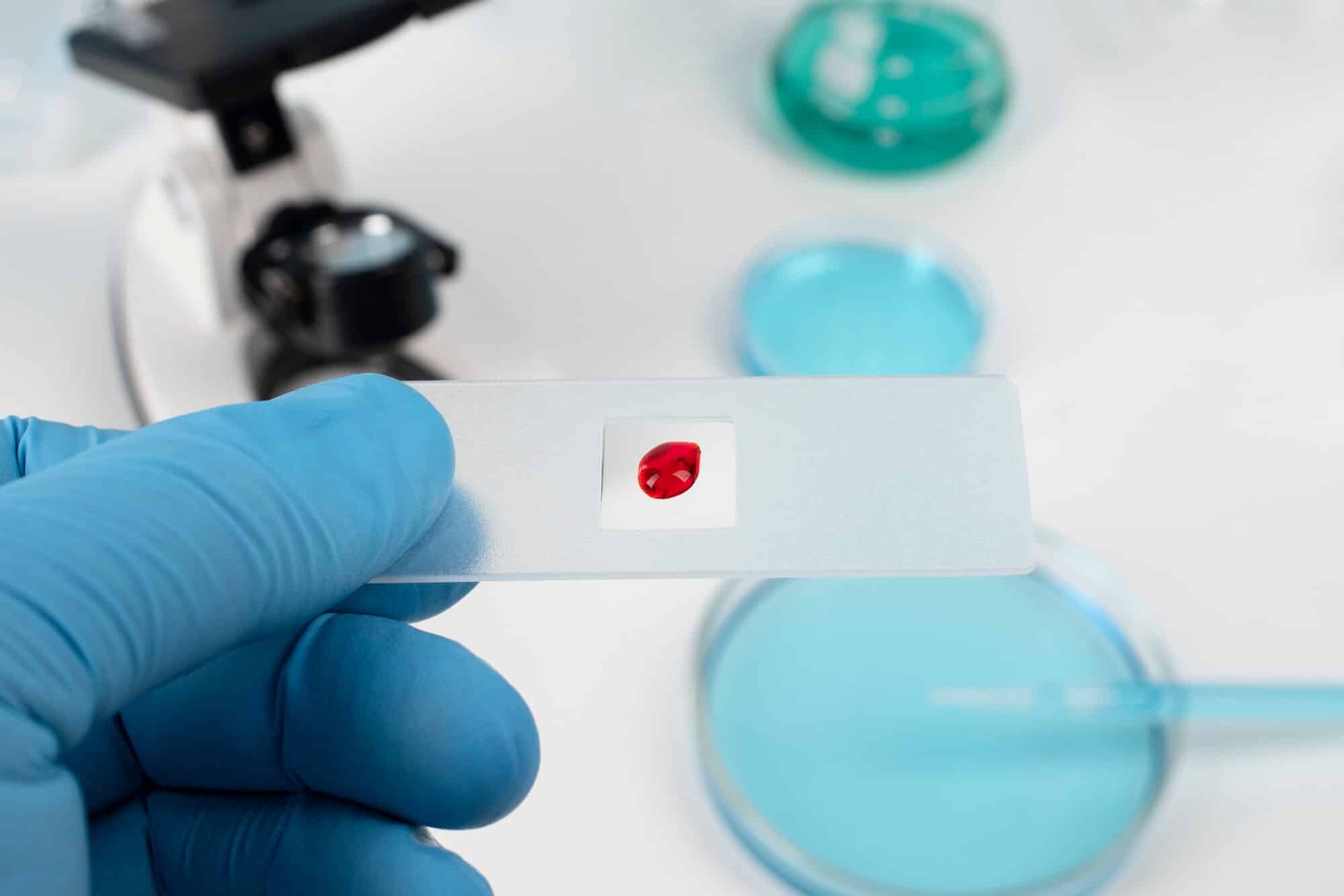
If you’ve been exposed to trichomoniasis or are showing symptoms, you should get tested as soon as possible. The infection can be detected through urine and swab tests, using a microscope or more advanced methods like a nucleic acid amplification test (NAAT) or a rapid antigen test. If you test positive for trichomoniasis, your healthcare provider may test you for other STIs to ensure you receive the right treatment.
Treatment for Trichomoniasis
Treatment of trichomoniasis involves taking antibiotics, such as metronidazole or tinidazole, for 5 to 7 days. You should abstain from drinking alcohol while taking the medication, as the interaction between the two can cause severe nausea and vomiting. You should also stop having sex until your treatment is complete to avoid spreading the infection.
Prevention Strategies for Trichomoniasis
Prevention of trichomoniasis protects you and your sex partners from infection. Here are some effective safety measures that you should follow:
1. Consistent use of condoms and dental dams
Always use latex or polyurethane condoms during sexual intercourse. For oral sex, use dental dams to create a protective barrier between the mouth and genitals. Trichomoniasis is highly contagious through skin contact, so protection should be used when engaging in any sexual activity.
2. Regular STI testing for high-risk individuals
You should get tested regularly for trichomoniasis and other STIs if you have multiple sexual partners and are unaware of their sexual history or if you engage in unprotected sex on a regular basis. Regular testing can catch the infection in its early stages and prevent complications.
3. Open communication with sexual partners
You should talk about sexual safety with your sex partners before becoming intimate. Share your STI history (if you have one) and ask them to do the same. If you find out that you have trichomoniasis, let your recent sex partners know so they can get tested too.
Get Treated for Trichomoniasis at Equality Health
Sexual health problems can weigh heavily on your mind and take a toll on your intimate relationships. Many people with STIs suffer in silence and delay getting tested out of embarrassment or fear. At Equality Health, we understand these challenges and offer discreet testing and personalized treatment in a caring, non-judgmental setting. Our healthcare professionals will walk you through each step of the process so that you can make informed decisions about your sexual health. Make an appointment today, and let us help you regain your peace of mind.
Frequently Asked Questions (FAQs)
Without medical treatment, trichomoniasis is unlikely to go away completely. You’ll need proper antibiotics prescribed by a doctor to get rid of the infection and avoid passing it on to others.
Yes, getting trichomoniasis again is possible and fairly common if your partner isn’t treated along with you. This is why doctors always recommend that both partners get treated at the same time, even if one person has no symptoms.
Untreated trichomoniasis can make you more vulnerable to other STIs, cause pregnancy complications, and lead to pelvic inflammatory disease.